
In early 2021, Brian O’Sullivan felt like he had made it through the pandemic relatively unscathed. He hadn’t gotten COVID-19, and like many others that year, he made a New Year’s resolution to take better care of himself. A routine physical and blood test seemed like a smart move. But the abnormal results that followed changed the course of his life.
His white blood cell count was high—16.1 when it should have been under 11. When retested 30 days later, the number was even higher. His doctor referred him to a hematologist, a term Brian wasn’t familiar with. A quick Google search revealed what he feared: hematology and oncology. “This is where it all ends,” he thought. “I’m going to die.”
The Diagnosis No One Sees Coming
Brian felt fine, which made the news even harder to accept. His doctor suspected chronic lymphocytic leukemia (CLL), a more manageable form of blood cancer. But further testing revealed a rarer, more aggressive diagnosis: mantle cell lymphoma (MCL). Brian was only 49—much younger than the typical patient.
“I got the news from a LabCorp notification on my phone,” he recalled. “It started my love-hate relationship with technology.”
In shock and panic, Brian turned to Facebook and found support groups for MCL patients. There, he realized something powerful: “I’m not alone in this.”
More Than Physical: The Mental Burden of a Rare Disease
Like many newly diagnosed rare disease patients, Brian wrestled not only with the physical reality of the disease but also with the emotional toll. His cancer included a TP53 gene mutation—a fact he initially blamed himself for. “I thought maybe this was karma for something in my past,” he said. “I was up at 3 a.m. most nights trying to figure out what I did wrong.”
That fear didn’t exist in a vacuum. Mantle cell lymphoma is often diagnosed at later stages and doesn’t always produce symptoms early on. “Cancer isn’t just physical,” he said. “I didn’t understand how much it would affect my mind until I was living it.”
A Devastating Insurance Denial
After finding a top specialist at Hackensack Meridian Health, Brian was encouraged by the possibility of a new kind of targeted therapy—BTK inhibitors (a class of drugs used to treat certain types of B-cell cancers) that could be more effective and less toxic than traditional chemotherapy.
But when it was time to begin, his insurance denied coverage.
“I thought that was it. I wasn’t going to die because there wasn’t a treatment—I was going to die because I couldn’t access it,” Brian said.
The insurance rejection letters continued to pile up. His blood counts got worse. “I was a number on a spreadsheet. That’s what it felt like,” he said.
A Clinical Study Becomes a Lifeline
A fourth oncologist offered hope. Brian was referred to Dr. Kumar at Memorial Sloan Kettering, who was leading a clinical study using similar medications to the ones Brian had been denied.
Brian feared more rejection—but on February 3, 2022, he was accepted into the study. “You matched everything. You can start healing today,” Dr. Kumar told him.
“I started crying,” Brian said. “Eighty-five percent of the depression I’d been carrying just left my body in that moment.”
As Brian progressed through the clinical study, Dr. Kumar became more than just his oncologist—she became a great friend.

Treatment That Worked—and Changed Lives
Brian began treatment with infusions and oral medications. Within one day, his white blood cell count dropped from 206 to 131. Over the next two years, he remained active in the study and continued to improve. Today, he’s no longer on medication—but continues with routine follow-ups.
The medications are now approved for widespread use. “I’ll never say I’m glad I got cancer,” Brian said, “but I know my participation in the clinical study helped push this treatment forward. Clinical studies saved my life—and they’re saving others now, too.”
Turning Pain into Purpose: Brian’s Mission
Since beginning his treatment, Brian has become a passionate patient advocate. He has spoken at events for the Leukemia & Lymphoma Society, met with New Jersey lawmakers, and visited Capitol Hill to discuss barriers to care and the need for more clinical studies.
Brian also created a Facebook group that began as a personal blog documenting his journey with MCL. Over time, he realized it wasn’t just his story—many others were on a similar path. Now, he uses the group to share not only his experiences but also to highlight the triumphs of fellow patients. What started as a personal outlet has grown into a supportive community of almost 3,000 members. “It’s not about being an influencer,” he said. “It’s about showing people that stage four isn’t the end.”

The Bigger Picture: Access for All
Brian is especially outspoken about step therapy—the insurance practice that requires patients to take and fail older, less effective treatments before covering newer ones. “Why should someone’s access to life-saving treatment depend on their income or insurance plan?” he asked. “Everyone deserves the most effective treatment, not just those who can afford it.”
His advocacy is personal—but it’s also about something bigger. “I don’t want just to survive. I want to help someone else survive, too,” he said.
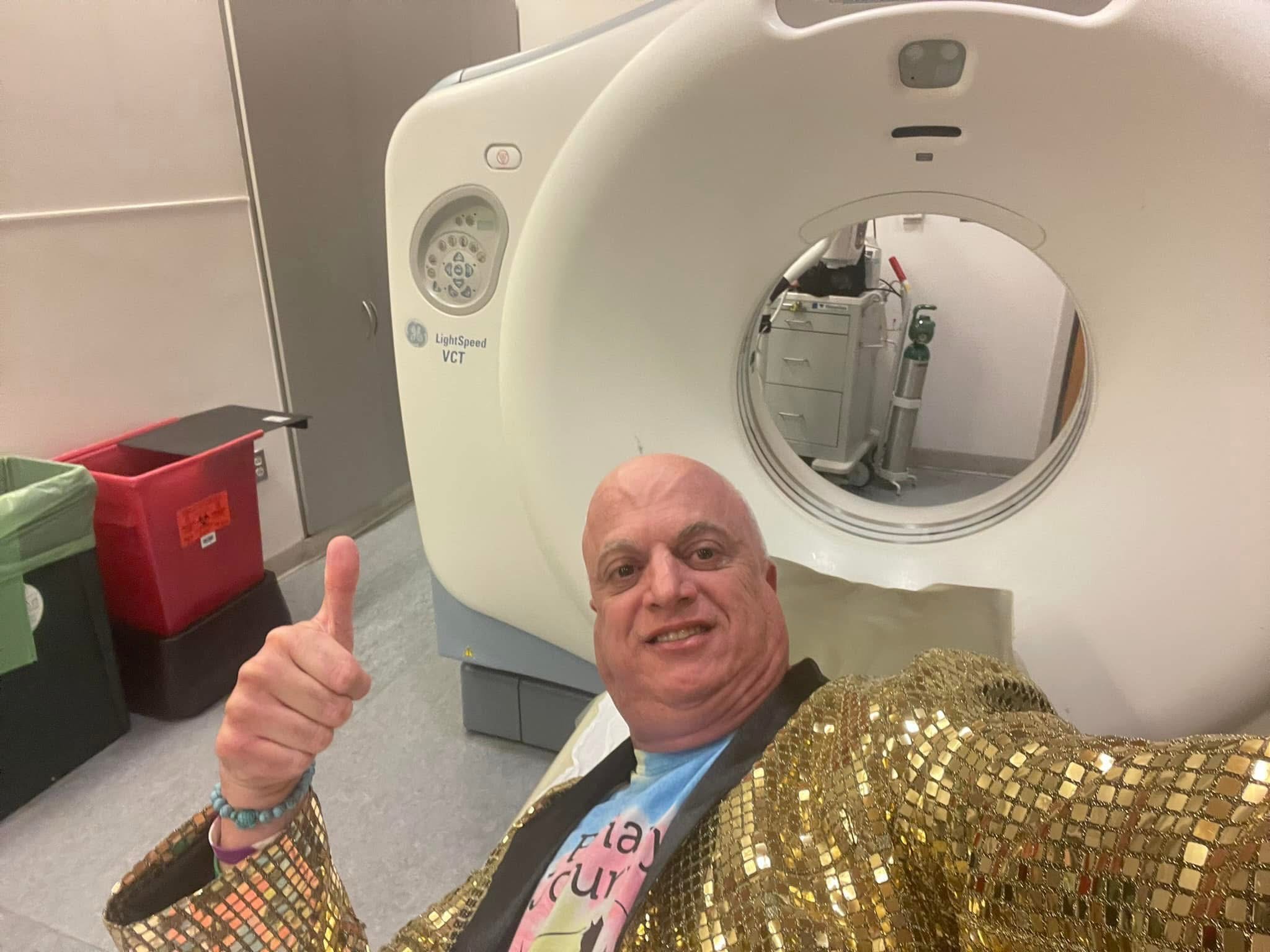
Brian knows his journey isn’t over. He still gets nervous before scans and still has hard days. But he also has purpose—and hope. “I hope to have scan-xiety for years to come,” he joked. “Because that means I’m still here.”